Frequently asked questions about hyperventilation

In this article you will find frequently asked questions and answers about chronic hyperventilation. The answers are put together with care. If your question is not listed, please contact us via the contact form. Click on a question to read the corresponding answer.
QUESTIONS AND ANSWERS
Getting a black-out from a hyperventilation attack is very rare. Usually it goes no further than dizziness and a (sometimes extreme) light feeling in the head. More often an imminent feeling of loss of consciousness rather than people actually getting a black-out. It does occasionally occur, but only in extreme situations and due to extreme anxiety.

with hyperventilation attacks
Breathing in the bag or putting your hands in front of the mouth to prevent the loss of carbon dioxide only works with acute hyperventilation. This is the form in which one suddenly breathes violently through a certain (anxious) situation. In these situations the carbon dioxide buffers (HCO3 ions) cannot compensate quickly enough. You can then - by the above method - limit the loss of carbon dioxide.
It does not help people with chronic hyperventilation nor does it function as a therapeutic medium. The respiratory center is not affected by these methods. And the attacks, where the bag can still help - are usually only present in the beginning of the hyperventilation syndrome. There is also a little device - called the HyperFree - that has about the same effect.
Chronic hyperventilation can be diagnosed as follows:
- Blood test for plasma bicarbonate levels. In people with chronic hyperventilation, these are usually (far) below the normal values. This type of research is not used that often.
- Saturation test. This type of test is quite popular with many GP's because it can be done immediately in the consulting room. A jab is put in a finger and a drop of blood is taken. In that drop the saturation (= saturation of the blood with oxygen) is measured. In our opinion, this type of research is not really reliable for diagnosing chronic hyperventilation.
- Capnographic tests. In this type of examination - by a pulmonologist - the amount of CO2 (= carbon dioxide) and O2 (= oxygen) in the exhaled air is measured. Both in the resting situation as after a hyperventilation provocation. By measuring the differences, it can be determined whether or not someone hyperventilates chronically. For this type of research you need a referral from the GP.
- ElektroMyoGram (EMG) focused on latency tetany. Latency tetany is a medical term for chronic hyperventilation. This type of test is very reliable. The test is done by specialized neurologists. It works as follows: An electrode is placed in the muscle of the hand between thumb and forefinger, which is connected to a sensitive measuring instrument. Then the blood circulation to the arm is temporarily inhibited with a band. At the moment the band is released, a hyperventilation provocation is done. This almost always leads to immediate cramping of the muscle with the electrode in people with chronic hyperventilation. The EMG then presents a number of characteristics. These characteristics are caused by, among other things, the lactic acid deposition on that muscle. You will also need a referral from the general practitioner for this type of examination. Note that this test can only be done by a specialized neurologist.
Conclusion: If you want to have chronic hyperventilation tested, preferably request a capnographic test or if possible an EMG.
Due to chronic hyperventilation, the respiratory center has been accustomed to a low acidity. The combustion processes continuously release CO2 (= carbon dioxide). The respiratory center has to correct the carbon dioxide level by triggering the respiration. The yawning, sighing and coughing are ways that people unconsciously use to exhale CO2 more quickly and to keep the breathing center "satisfied".
What can you do about it?
You can unlearn these sighs. Every time you start to sigh, catch the exhalation by allowing the air to slowly escape. You hold your lips together and slowly exhale through the closed lips. The air then slowly escapes and thus less CO2 is lost. This is something that you have to teach yourself. If you have done it often enough, it becomes a reflex (= an automatism) and you do not have to think about it anymore.
Yawning is not all bad, because it also brings relaxation. However, you lose a lot of CO2 by yawning. You can use a similar method as above to unlearn the yawning.
In a complex organism such as the human body everything influences each other. In a premenstrual syndrome (PMS) situation you can certainly suffer more from the hyperventilation symptoms. And in chronic hyperventilationyou can certainly suffer more from the symptoms of PMS. This is not to say that there is a causal link between the two, but rather an interaction where one reinforces the other.
The chronic hyperventilation creates a less acidic environment in the brain. Therefore also the hormonal balances can be disrupted. The hormone system is coordinated by the pituitary gland and hypothalamus, two organs in the brain. For example, a disordered hormone balance can manifest itself through symptoms of PMS or hypoglycaemia (= shortage of sugar). The production of adrenal hormones, such as stress hormones or cortisol, can also be disrupted. You also often see this in a burn-out..
The hormones regulate many processes in the body. The symptoms that arise depend on the total health and genetic disposition of the patient. One cause, such as a less acidic environment in the brain, can have totally different hormonal consequences for different people. And that makes it very difficult for both the doctor and the patient to explain the relationship between the experienced symptoms and the cause of these symptoms.
Muscle pain, cramps and similar sensations are causes by chronic hyperventilation. They happen because the lactic acid metabolism is out of order. The muscles try to compensate for the shortage of carbon dioxide in the organism. They release lactic acid. This leads to muscle aches and cramps. Or involuntary muscle twitches, such as an eyebrow that vibrates uncontrollably.

If we are anxious, we hyperventilate. It is a normal reaction of our body. The body compensates for the loss of carbon dioxide by the buffer systems in our blood. Primarily, therefore, fear is the cause and not the effect of hyperventilation. But we can also hyperventilate because of stress. Then the fear component is not immediately present. It is only during the first hyperventilation attack that fear comes to the surface. The fear in this situation seems to be a consequence rather than a cause.
Cause and effect turn around!
The annoying thing about the syndrome of chronic hyperventilation is that the symptoms caused by it often make people extremely frightened. People start to doubt their own body. This increased anxiety further drives the respiratory center. Now the fear has become the cause! Breaking the vicious circle fear > hyperventilation > more fear is one of the most important aspects of curing the hyperventilation syndrome. By understanding what hyperventilation is and what it does in our body, the fear can be reduced and often even eliminated. And then all that remains is to reset the respiratory centers sensitivity for carbon dioxide.
The blood has a certain acidity. That acidity is expressed (in chemistry) in pH values. The pH scale is a logarithmic scale ranging from 0 to 14. Lower than 7 means that the solution is acidic. The lower the value, the more acidic it is. Above 7 means that the solution is alkaline. Values below 0 and above 14 are possible, but only in extreme situations. Such substances are generally very dangerous: concentrated acids and concentrated alkalis.
The pH or acidity of human blood is - normally - between 7.3 and 7.5. So a little on the alkaline side. This value is kept within these narrow limits under various conditions. For this purpose are the so-called buffers in the blood. A buffer is a substance that is capable of absorbing changes in the H- or OH-ion concentration, without this leading to changes in acidity. Among the buffers in the blood we can count the bicarbonate system, the plasma proteins and certainly not the least important thing, the blood dye. The collective capacity of the various buffers in the blood to maintain the correct acidity is called the buffer capacity.
If the pH limits of the blood are exceeded despite the various buffer systems, serious situations occur. If the pH drops too much an acidosis / acidification occurs. If the pH rises too much, alkalosis occurs. Changes in breathing (respiration) may cause the carbon dioxide to rise or fall. An increase in the carbon dioxide leads to an increase in the bicarbonate. This condition is called a respiratory acidosis. A decrease in the carbon dioxide leads to a decrease in the bicarbonate. This condition is called respiratory alkalosis (= hyperventilation).
With a hyperventilation provocation test, the doctor lets you consciously hyperventilate for a few minutes by allowing you to breathe heavily. In people with chronic hyperventilation there is not enough buffer to pass this test without producing the hyperventilation symptoms. The acidity decreases and the range of symptoms occurs. That is a clear indication to the doctor that you suffer from the hyperventilation syndrome. The disadvantage of this test is that you can be quite upset for a long time. In our opinion, the tests mentioned in question 3 are a little more patient-friendly.

in chronic hyperventilation
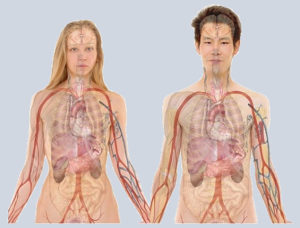
Fatigue is inherent to chronic hyperventilation. The blood is usually alkaline. Because of that the red blood cells can not deliver their oxygen properly to the tissues. In addition, the blood vessels are narrowed so there is no good blood flow. This creates the extreme feelings of fatigue. The bodily functions are severely impacted.
Incidentally, 12 hours of sleep per day is not the solution. It is much better to give the body a routine of 8 hours of sleep per day. Try to always sleep at the same time and get up at the same time. See for more information about this the article about a healthy lifestyle. Try to go to sleep well before 12 o'clock PM.
Most people develop - by experiencing the Symptoms of chronic hyperventilation over a longer period of time - hypochondriacal (= fear of illness) symptoms. The reason for this is that you no longer trust your own body. Eventually that leads to the development of all kinds of hypochondriacal fears. Very well known are the fear of heart defects, serious diseases such as cancer and tumors. It is in fact a logical consequence of the fact that we experience a range of symptoms because of chronic hyperventilation. There is something wrong with us but we do not know what causes it. So it is logical that we start distrusting our body...
These fears excite the respiratory center even more and the hyperventilation symptoms get worse. Also because of the lack of buffer. This is one of the vicious vicious circles in which you end up with hyperventilation. The solution lies in breaking this vicious circle. That is why it is so important to understand what is wrong with you and how the mechanism of chronic hyperventilation works.
In principle, chronic hyperventilation is not hereditary. But children consciously and unconsciously pick up many things from their parents. In addition, character traits are genetically determined. If these character traits promote chronic hyperventilation, the child therefore more or less has a genetic predisposition to hyperventilation. If a parent is anxious, the (young) child automatically becomes too. The child feels that. In this way - often at a very young age - the basis is laid for the development of the chronic hyperventilation syndrome! In practice, we see that children whose parents suffer (or have had) chronic hyperventilation, often later also develop hyperventilation symptoms. For a more detailed explanation of this, read the article on the the psychological profile of the patients.
Chronic hyperventilation exists in many grades. You can be heavily affected. You suffer from hyperventilation attacks, continuous misery, fears, phobias. You can have occasional periods where the symptoms show up. Especially in busy periods and stressful situations. It all depends on the setting of the respiratory center. You could, as it were, think of a scale of the extent to which someone suffers from chronic hyperventilation:
 |
|
 |
|
 |
|
 |
|
 |
|
All intermediate values are possible. People with hyperventilation symptoms are somewhere between 50 and 100 on this scale. The HyperVen therapy takes you in the direction of 1 on this scale.

There are no medicines for chronic hyperventilation. However, there are medications that exert a favorable influence on anxiety and stress, but the hyperventilation usually remains. The medications that are commonly prescribed are antidepressants. Your doctor or pharmacy can give you more information about this. See also the article on medicine use with chronic hyperventilation.
It is best to treat chronic hyperventilation at the source, namely to reset the respiratory center in the brain to a higher CO2 tolerance. For this purpose Ph.D. Snitslaar developed The HyperVen therapy.
Dizziness and the feeling of imminent fainting are very common in chronic hyperventilation. It is caused by the shortage of blood that the brain receives. The reason for this is that the blood vessels in people with chronic hyperventilation are constricted. The shortage can amount to about 40%! The deeper you are in the chronic hyperventilation syndrome, the worse the light feeling in the head becomes.
There may of course be other causes for dizziness or feelings of imminent fainting. It can also be an indication of Ménière's disease (an equilibrium disorder). If in doubt, request a diagnosis of chronic hyperventilation. Chronic hyperventilation is easy to test for. If you experience a feeling that everything starts to revolve around you, then going to the doctor is absolutely essential.

and chronic hyperventilation
Stress and chronic hyperventilation often (usually?) go hand-in-hand. There is a clear relationship between stress and hyperventilation. In the first instance, stress is often the trigger for hyperventilation. After a few months the buffer systems in the blood will be used up. Then the symptoms of both stress and hyperventilation arise. We become worried and our nervous system reacts with fear. Fear sets the respiratory center to increased activity and that results in a further increased hyperventilation. This increases the symptoms and anxiety. And that makes the hyperventilation worse. This often leads to a hyperventilation attack.
Stress comes - just like hyperventilation - in all kinds of degrees. During rest (sleeping > dreams) our nervous system starts to process stress (releasing stress) and during (busy) activity we accumulate new stress. If we accumulate more stress than we can process in our dreams and rest periods, the stress goes out of balance. This build-up can go on for long time. But in the end our subconscious mind can no longer store any more stress and the stress begins to penetrate the consciousness mind. If this accumulation of stress is extreme, we call it a burn-out. Also traumatic experiences can exert tremendous stress build-ups.
Stress causes symptoms that are very similar to the symptoms of chronic hyperventilation. The combination is actually quite bad. Our nervous system must handle both the stress and the hyperventilation symptoms. And that takes its toll from our mental stamina.
A few points of attention for reducing stress:
- Make sure you do not accumulate more stress than you can handle. That is not an easy thing to do, as it cannot be expressed in numbers. But usually people have a fairly good idea of the amount of stress they are confronted with every day. Make sure this is not excessive.
- Provide adequate (night) rest
- Sport regularly, but not excessively. Sport is a form of mental relaxation that releases and dissolves stress
- Be careful with the consumption of alcohol
See also the article about a healthy lifestyle.
Chronic hyperventilation does not happen to you suddenly. It is the gradual reduction of the buffer systems that eventually leads to the hyperventilation syndrome. You will hardly notice anything as long as the buffers can still compensate. When the buffers are depleted, the blood becomes alkaline and then suddenly a whole array of symptoms occur. This usually results in the first hyperventilation attack. People find it difficult to relate the period in advance to the attack, but in fact it has been going on for a long time.
Once the buffers are depleted and the respiratory center has become accustomed to the new situation with low buffers, the breathing center automatically maintains chronic hyperventilation. And that can go on for years. For some people even their whole life...

due to chronic hyperventilation
The imagined fears of diseases are called hypochondriacal fears. These are quite common in people with chronic hyperventilation. Mostly they relate to our heart, tumors, diseases like cancer, cerebral haemorrhages and so on. The common denominator is of course our fear of death, which forms the basis for all other fears.
These fears often arise because people do not know where the symptoms come from. Also often because the doctor 'can not find anything'. We do not feel well, but we do not know what is going on. As a result, we lose confidence in our own body. And that is usually the basis of the hypochondriacal fears.
The fears can also develop into phobias. This is because people get the same symptoms every time in the same situations. Then one starts to avoid those situations. Because we are afraid of the symptoms, we rather avoid the situation than having to endure the uneasy feelings. Well-known examples of these are: the queue for a cash register, the cinema, a square with many people, elevators. Many people even develop a so called street phobia...
Is avoiding these phobic situations better than going through them?
There are different opinions about this. On the one hand, the avoidance behavior confirms that one is no longer able to deal with a certain situation. And that is psychologically spoken not healthy. On the other hand, forcing yourself to endure those situations, can lead to an escalation of the hyperventilation symptoms. So it depends on the degree of your hyperventilation syndrome. If you have very little to no buffer to compensate for the stress of that situation, then forcing yourself can lead to a severe aggravation of the symptoms.
Our advice is to first provide more carbon dioxide buffers with The HyperVen therapy. Once you have made some progress, you can try (but be careful) to expose yourself to the phobic situations again. If you then experience the symptoms do not come up, confidence in your body and yourself will grow again. The phobic avoidance behavior will then eventually die out.
The short of breath feeling is caused by the respiratory center. It has been accustomed to a low acidity in the blood. With a slight increase in acidity, the respiratory center immediately triggers inhaling. This will make you breathe too quickly. The trigger to inhale comes when you exhale. And that makes you feel short of breath.
In addition, the blood vessels are narrowed because of the low acidity of the blood. As a result, the oxygen supply to organs and tissues is reduced. On top of that the red blood cells cannot properly deliver their oxygen in an alkaline environment. The brain records the deficiencies. These three factors aggravate each other. Together they intensify the short of breath feeling.
